COVID-19: Transmission modes and measures to prevent and control risk, including the role of ventilation
Last update in French: May 19th 2022.
Frequently asked questions
- Is COVID-19 transmitted through the air?
- Can airborne transmission of the virus occur over long distances?
- Are there specific conditions that support aerosol transmission at a distance of 2 meters or more?
- Certain environmental parameters influence the survival of SARS-CoV-2 in indoor environments. What are they?
- Given that the virus is transmitted by aerosols in close proximity, how can we protect ourselves from getting COVID-19?
- What role does ventilation of indoor environments play in spreading the virus?
- What is the difference between ventilation and air filtration?
- Are these ventilation and filtration measures effective in limiting the transmission of the SARS-CoV-2 virus?
- Can portable air filtration devices reduce the transmission of SARS-CoV-2?
- Can natural ventilation measures be effective in reducing the risks of virus transmission?
- Have the recommendations for the aeration and ventilation of indoor public spaces changed, or should they?
- When hospitals, CHSLDs, and schools have outdated heating and ventilation systems, what can be done to protect occupants?
- What are the INSPQ'S recommendations for protecting healthcare workers in healthcare settings, given the risk of transmission by aerosols?
Is COVID-19 transmitted through the air?
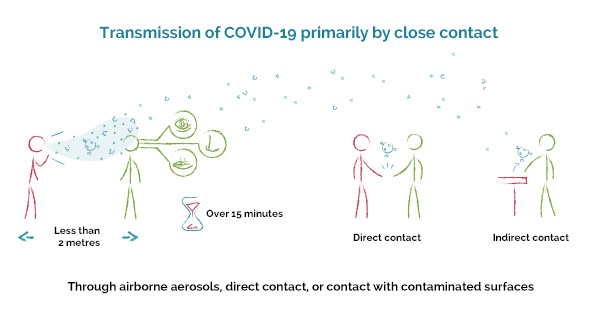
SARS-CoV-2, the virus that causes COVID-19, is primarily transmitted through close contact between people who are less than 2 metres apart for more than 15 minutes. This transmission occurs in part through aerosols in the air.
However, it is difficult to ascertain exactly how transmission occurs in close proximity, since it may be caused by direct contact, aerosols in the air, or contact with a surface contaminated by respiratory particles from an infected person. For aerosols in the air, there is a continuum of respiratory particles of different sizes that may contribute to transmission.
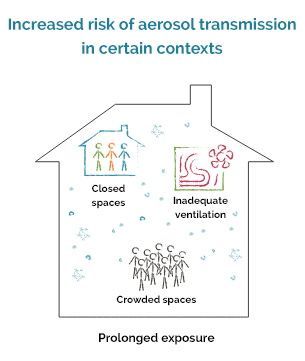
The risk of transmission of SARS-CoV-2 is also increased in closed, crowded, inadequately ventilated spaces with prolonged exposure. In these specific conditions, the maximum distance at which one can be infected remains unclear, but it is unlikely to be more than a few meters.
Can airborne transmission of the virus occur over long distances?
At present, there is no direct evidence that the virus is airborne, that is to say that it is transmitted in the air over distances of more than a few meters, as is the case for other contagious diseases like measles or tuberculosis. Instead, according to current knowledge, SARS-CoV-2 is primarily transmitted in close proximity by respiratory particles of various sizes that contain the virus.
Are there specific conditions that support aerosol transmission at a distance of 2 meters or more?
The risk of transmission of SARS-CoV-2 is increased in closed, crowded, inadequately ventilated spaces with prolonged exposure, i.e. more than 15 minutes. Studies suggest that air currents between people in enclosed spaces may also be associated with transmission at more than 2 metres.
Certain environmental parameters influence the survival of SARS-CoV-2 in indoor environments. What are they?
The INSPQ has studied the viability of the virus in indoor environments.
Laboratory studies have shown that the airborne presence of the SARS-CoV-2 virus is favoured at a temperature 4°C and relative humidity of 20 to 40%. These same studies have shown that the virus can survive in the air and on surfaces from a few minutes to a few hours, depending on the environmental context.
Given that the virus is transmitted by aerosols in close proximity, how can we protect ourselves from getting COVID-19?
Implementing a combination of preventive and protective measures makes it possible to limit the transmission of SARS-CoV-2, whether in the community, at the workplace, or in healthcare settings. These measures include:
- Limiting contacts
- Physical distancing
- Respiratory hygiene and etiquette
- Hand hygiene
- Adequate indoor ventilation
- Mask-wearing
- Cleaning and disinfecting the objects and surfaces of the environment
- Routine practices and additional precautions for preventing the transmission of infections as recommended for healthcare settings
What role does ventilation of indoor environments play in spreading the virus
Preventive measures such as reducing contacts, physical distancing, hand hygiene, respiratory hygiene and etiquette, cleaning and disinfection, physical barriers, medical masks, and other types of masks are known to play a role in limiting the transmission of the SARS-CoV-2 virus.
Proper ventilation contributes to better air quality and helps prevent the accumulation of potentially infectious particles in indoor spaces.
It is important to work with ventilation system professionals. They will ensure you opt for ventilation solutions whose impact has been assessed and is suitable to the context.
What is the difference between ventilation and air filtration?
Ventilation and filtration are both elements that can be included in a combination of control measures to prevent the transmission of SARS-CoV-2 in indoor environments.
Ventilation consists of extracting indoor exhaust air from an environment and diluting the contaminants therein by introducing air from the outside. Indoor environments can be ventilated by mechanical systems or by opening windows.
The suction capacity of the mechanical ventilation systems in most buildings is insufficient to capture drops and larger aerosols in the indoor environment, as they tend to rapidly fall to the ground.
Mechanical filtration involves the use of filters designed to capture particles in the air. These filters can be inserted in a ventilation system or a portable filtration device.
Are these ventilation and filtration measures effective in limiting the transmission of the SARS-CoV-2 virus?
It is generally accepted that proper ventilation of indoor environments is an effective measure for managing indoor air contaminants. Mechanical ventilation systems can help extract and dilute gases and fine particles, and other contaminants suspended in the air. Ventilation systems must be well designed and properly installed, maintained, and used in order to be effective.
Filters can be installed in a ventilation system to reduce particles in the recirculating air. When properly selected, positioned, maintained, and used, they may contribute to reducing the concentration of viral particles in indoor air.
Can portable air filtration devices reduce the transmission of SARS-CoV-2?
In some situations, portable air purifiers equipped with HEPA filters may be a complementary means to reduce the infectious load in indoor air. However, there is insufficient evidence that these devices contribute to either reducing or increasing the transmission of respiratory diseases.
It is therefore important to work with ventilation and filtration system professionals and not opt for air filtration devices whose impact has not been fully analysed and that may not be suitable. Ventilation and filtration systems must be well designed and properly installed, maintained, and used in order to be effective.
Use of ventilation should be recommended in combination with other protective measures such as physical distancing, minimizing contacts, and use of respiratory hygiene. The complementarity of all these control measures reduces the risk of COVID-19 transmission in indoor environments.
Can natural ventilation measures be effective in reducing the risks of virus transmission?
A room can be naturally ventilated by opening windows or doors to the outside. Natural ventilation occurs through the difference in air pressure between a building’s interior and exterior, as the air moves from high-pressure areas toward low-pressure areas. However, the effectiveness of this ventilation practice varies as the difference in pressure can be modulated by a number of factors, including the difference in temperature between the indoor and outdoor air; the presence or absence and direction of air currents; the type, number, and layout of windows; etc.
In the case of some buildings that are not equipped with mechanical ventilation systems or that cannot supply the recommended volumes of fresh air, intentional natural ventilation can be an option worth considering or using as a complement. However, the effectiveness of this type of approach for exchanging indoor air in a given environment remains conditional on good understanding of the elements that could hinder or facilitate the flow of air in the building (architecture of the premises, presence of obstacles, interaction with different mechanical systems, etc.).
Different options (e.g., a combination of measures) can be considered regarding natural ventilation. These options should ideally be assessed according to the specific characteristics of the building concerned and its occupants.
It is also recommended that this natural ventilation be carried out for 10-15 minutes, at least twice a day, and also at strategic times (during breaks, during meals, etc.).
Have the recommendations for the aeration and ventilation of indoor public spaces changed, or should they?
The CNESST's recommendations maintain that premises that cannot be ventilated should not be occupied by workers. These recommendations are in the Regulation respecting occupational health and safety (Article 101 and following articles, Division XI). The standards for air changes per hour for each setting have been clearly set out. Specific suggestions for the maintenance of ventilation systems for SARS-CoV-2 have been put forward, but the maintenance and evaluation of systems must always be supervised by a professional.
When hospitals, CHSLDs, and schools have outdated heating and ventilation systems, what can be done to protect occupants?
Firstly, ensure compliance with barrier measures, both individual (particularly physical distancing), and environmental (for example, installing Plexiglass). In other words, it is essential to ensure individual protection and limited contacts. If these measures are respected, outbreaks can be limited in these settings.
That being said, ventilation systems are very complex. Professionals are responsible for the ventilation in different environments such as hospitals, schools, and other public buildings. It is important to involve these specialists, so that they can optimize the ventilation systems already in place to meet the standards for the specific use of the setting.
What are the INSPQ'S recommendations for protecting healthcare workers in healthcare settings, given the risk of transmission by aerosols?
Respecting all preventive and protective measures remains crucial in controlling SARS-CoV‑2 transmission and outbreaks, both in healthcare settings and other settings. No single measure is 100% effective on its own.
Ensuring proper ventilation in all care facilities is important. This involves a good knowledge of the systems in place and identification of areas where ventilation must be improved. It is important to work with ventilation system professionals.
Wearing an N95 respirator is recommended in some situations that may increase the risk of transmission, such as during aerosol-generating medical procedures. It can also be considered in other circumstances, such as uncontrolled outbreaks in healthcare settings. The Comité sur les infections nosocomiales du Québec (CINQ) is continuing its work with a view to adapting the recommendations for wearing personal protective equipment as needed as the scientific knowledge on COVID-19 evolves.