Operating Room with a Suspected or Confirmed COVID-19 Case: Interim Recommendations
Note that the information herein is based on the scientific evidence available on the date of this statement. Several questions on operating room setup for suspected and confirmed cases of COVID-19 have come from these facilities. Below are the measures to implement.
Preparatory Measures
- Postpone all elective surgeries (for at least one month) and if possible, postpone urgent surgeries until the case is no longer contagious or until a test rules out the possibility of COVID-19 for a patient with compatible symptoms.
- Prepare for all urgent surgery scenarios for suspected or confirmed cases of COVID-19 with the various teams: technical services, IPC, operating room, surgeons, anesthesiologists, etc.
- Determine whether the surgery has a high risk of generating aerosols (see below) by discussing with the surgeon.
- Favor epidural or locoregional anesthesia whenever possible as these cases will not have to be intubated the majority of the time (intubation being an aerosol-generating medical procedure [AGMP]).
- If possible, establish COVID-19-dedicated operating room(s) with independent ventilation systems separate from those of the other rooms. The ventilation system(s) must be equipped with filters.
- When possible, and without modifying the configuration of the ventilation system in the operating rooms, maximize the percentage of air vented outdoors, ideally up to 100%. Should it be impossible to vent 100% of the room air outside, increase the system’s filtration level to MERV 16, or ideally HEPA, to avoid contaminating the areas adjacent to the operating room (the efficiency of MERV 16 filters is similar to that of an N95 respirator).
- The operating room pressure must remain positive relative to the adjacent spaces; do not attempt to put it in negative or neutral pressure modes.
- Some procedures, such as intubation, will generate aerosols (AGMPs), regardless of whether the room is positively pressurized or negatively pressurized. For these procedures, personal protective equipment for additional airborne/contact precaution with eye protection, are necessary for the people present until the air is filtered or replaced (by air exchange).
- The pressure differential between two rooms (negative pressure or positive pressure) only influences the potential for contaminants to migrate from the positive pressure room to the negative pressure room.
-
Putting an operating room in negative pressure mode will cause uncontrolled air movement and permanently introduce large volumes of unfiltered air into the rooms (significant infection risk at the surgical level). For this reason, in the Canadian and American standards for designing ventilation systems in healthcare facilities, all operating rooms are positively pressurized and have been so for a very long time.
- The preferred method to ensure air containment in a positive pressure operating room is to have a negative pressure ventilated anteroom that intercepts the air leaving the room. An anteroom is required for all doors accessing the operating room that can be opened.
- Check that the doors are well adjusted so as to limit excessive air loss (note that doors are not designed to be perfectly sealed).
- To the extent possible, schedule the case for the end of the day or the evening, when there are fewer staff and patients in the operating room.
- If the surgical intervention requires intubation, consider performing the intubation outside of the operating room in a negative pressure room, if possible (e.g., a patient already in the ICU in a negative pressure room), and then transporting the intubated patient to the operating room. If the patient must be intubated in the operating room, the intubation ideally must be done without the surgical team in the room during this procedure, after which the surgical team must wait for the required change of air (if there are 15 air exchanges/hour, wait 30 minutes) before entering.
- A patient on droplet/contact precautions with eye protection in the patient care unit due to COVID-19 can be operated on with droplet/contact precautions and eye protection once the intubation step is complete and the waiting time has been respected (e.g., ankle ORIF), and if the surgical procedure is not a type that will generate infectious aerosols containing COVID-19.
- If the patient does not require intubation for the intervention, they must wear a procedure mask while being transported to the operating room as well as during any surgical procedure.
- To implement for the COVID-19-dedicated operating room:
- Once the patient is positioned in the operating room, lock all doors to this dedicated operating room except for one single access door (the one toward the anteroom) to avoid uncontrolled transfers of contaminated air.
- Display a sign on the access door to advise that the room is COVID-19-dedicated and that entry is prohibited except for requisite staff.
- In cooperation with technical services and in compliance with standard CSA Z317.2:19 Special requirements for heating, ventilation, and air-conditioning (HVAC) systems in health care facilities, install the two measures described below if possible. If both measures cannot be installed, prioritize measure No. 1.
1. A temporary anteroom (containment unit) in the corridor to the operating room. The anteroom will be under negative pressure relative to the operating room and to the corridor. It will be equipped with a HEPA filtration device (air capture in the lower part of the anteroom and output in the upper part of the anteroom and/or in the hallway). In the case of a permanent airlock, vent the air directly outside.
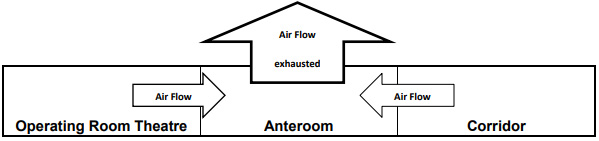
Image excerpted from Alberta Health Services. Best Practice Guidelines for Airborne Precautions in an Operating Room (2015).
2. A mobile HEPA filtration device directly in the operating room, set up to capture contaminated air close to the source. The exhaust airflow from the mobile HEPA filtration device must be vented away from the vertical laminar airflow protecting the patient, near an air return inlet if possible.
Surgeries with a High Risk of Generating Infectious Aerosols Containing COVID-19
- In some cases, the surgery itself may generate infectious aerosols containing the COVID-19 virus (e.g., ENT, transnasal and transoral, and maxillofacial procedures; skull base and pulmonary surgery) and is considered at high risk of generating aerosols (Patel et al.). It is always preferable to postpone the surgery. Respect all the principles listed above and measures No. 1 and 2, also listed above, should be in place. The surgery must be carried out in the evening or at night, if possible. For this type of surgery, even if the patient was on droplet/contact precautions with eye protection in the patient care unit, the intubation, extubation and entire duration of the surgical procedure must be carried out using airborne/contact precautions with eye protection.
- A request has been addressed to the Unité d’évaluation des technologies et des méthodes d’interventions en santé (UETMIS), which is the technology and healthcare procedure methods evaluation unit at CHU de Québec, to create a list of surgeries at high risk of generating infectious aerosols containing COVID‑19.
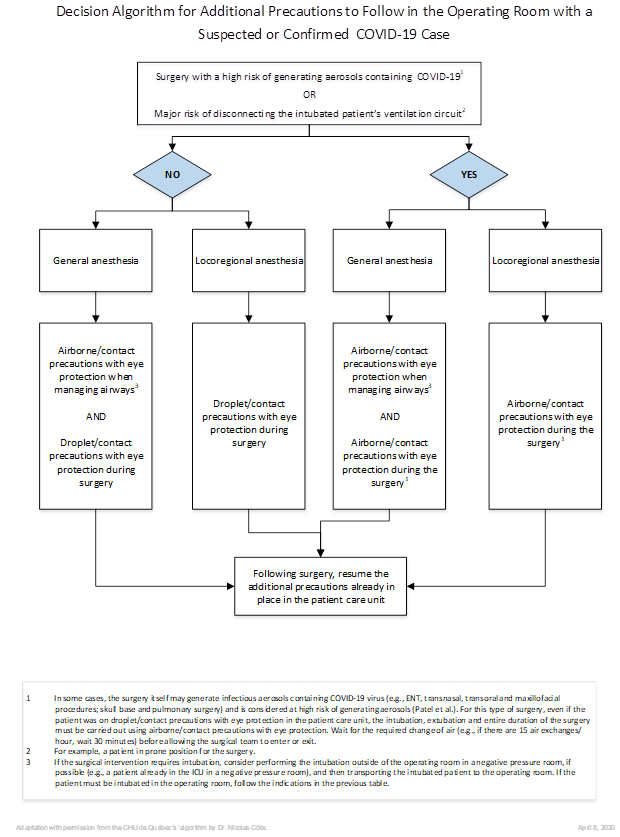
Specific measures according to the additional precautions already in place in the care unit and the type of anesthesia
| Type of surgery | Surgery with low risk of generating aerosols |
Surgery with high risk of generating aerosols |
||
|---|---|---|---|---|
|
Additional precautions in the care unit |
Droplet/contact with eye protection |
Droplet/contact with eye protection |
||
|
Type of anesthesia |
Local anesthesia |
General anesthesia |
Local anesthesia |
General anesthesia |
|
In the patient’s room/pre-op area |
If non intubated: |
If already intubated in the care unit: If intubation required: * Have a closed circuit and a filter with high filtering efficiency (e.g., those approved for tuberculosis) on the endotracheal tube or the expiratory end of the ventilator circuit. |
If not intubated: |
If already intubated in the care unit: If intubation required: * Have a closed circuit and a filter with high filtering efficiency (e.g., those approved for tuberculosis) on the endotracheal tube or the expiratory end of the ventilator circuit. |
|
Additional intra-op precautions |
Droplet/contact with eye protection (surgical mask) |
Airborne/contact with eye protection (N95 respirator) for all personnel present in the operating room |
||
|
Post-op/ recovery
Extubation |
Recovery |
Extubation |
Recovery The recovery room according to the additional pre-op precautions in place. |
Extubation In the operating room: the extubation must be done without the surgical team in the room during this procedure. Wait for the required change of air (e.g., if there are 15 air exchanges/hour, wait 30 minutes) before moving the patient from the room and allowing personnel and a new patient to enter. |
References
- Alberta Health Services. (2014). Best Practice Guidelines for Airborne Precautions in an Operating Room. Online: https://www.albertahealthservices.ca/assets/infofor/hp/if-hp-ipc-bpg-airborne-or.pdf
- American Society of Anesthesiologists. (2020-03-20). Online: https://www.asahq.org/about-asa/governance-and-committees/asa-committees/committee-on-occupational-health/coronavirus and https://www.asahq.org/about-asa/newsroom/news-releases/2020/03/update-the-use-of-personal-protective-equipment-by-anesthesia-professionals-during-the-covid-19-pandemic
- Centers for Disease Control and Prevention (CDC). (2003). Guidelines for Environmental Infection Control in Health-Care Facilities. Online: https://www.cdc.gov/infectioncontrol/guidelines/environmental/background/air.html#c5c
- Colorado Medical Society (CMS). CMS Adult Elective Surgery and Procedures Recommendations. Version 2020-03-15. Online: https://www.cms.gov/files/document/cms-non-emergent-elective-medical-recommendations.pdf
- Institut national de santé publique du Québec (INSPQ). COVID-19 : Mesures de prévention et contrôle des infections dans les milieux de soins aigus : recommandations intérimaires. Version 2020-03-20. Online: https://www.inspq.qc.ca/covid-19/milieux-de-soins.
- Nebraska Medicine. (2020). COVID-19 in procedural areas. Online: https://www.nebraskamed.com/sites/default/files/documents/covid-19/COVID-procedural-areas.pdf
- Patel et al. Avis Stanford.
- Public Health Agency of Canada (PHAC) and Canadian Lung Association. (2014). Canadian Tuberculosis Standards. Online: http://www.phac-aspc.gc.ca/tbpc-latb/pubs/tb-canada-7/index-eng.php
- Ti, L. K., Ang, L. S., Foong, T. W. & Ng, B. S. W. (2020). What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Canadian Journal of Anesthesia. Online: https://doi.org/10.1007/s12630-020-01617-4
- Vancouver Coastal Health. (2017). IPAC Best Practices Guideline – Airborne Precautions in the Operating Room. Online: http://ipac.vch.ca/Documents/Additional%20Precautions/Online/Airborne%20Precautions%20in%20the%20Operating%20Room.pdf
- Wax, R. S. & Christian, M. D. (2020). Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients, https://link.springer.com/article/10.1007%2Fs12630-020-01591-x
- Witterick I., President, Canadian Society of Otolaryngology-Head & neck Surgery. (2020-03-19). Online: https://www.entcanada.org/news-events/society-e-blast/
- Wong, J., Goh, Q. Y., Tan, Z., Lie, S. A., Tay, Y. C., Ng, S. Y. & Soh, C. R. (2020). Preparing for a COVID-19 Pandemic: A Review of Operating Room Outbreak Response Measures in a Large Tertiary Hospital in Singapore. Online: https://www.ncbi.nlm.nih.gov/pubmed/32162212?dopt=Abstract